Securing rights in healthcare

When someone’s capacity for decision making is compromised they can become vulnerable, marginalised and invisible.
By using philosophy to understand the complexities of care, Essex researchers are helping ensure everyone is recognised.
The Essex Autonomy Project is changing policy and practice by advising governments and hospitals, supporting activists and advocacy organisations, and training frontline professionals.

Applying philosophy to rights in care

In 2021-22 more than 50,000 people were detained under the Mental Health Act in England and the number of people living in UK care homes currently stands at more than 400,000.
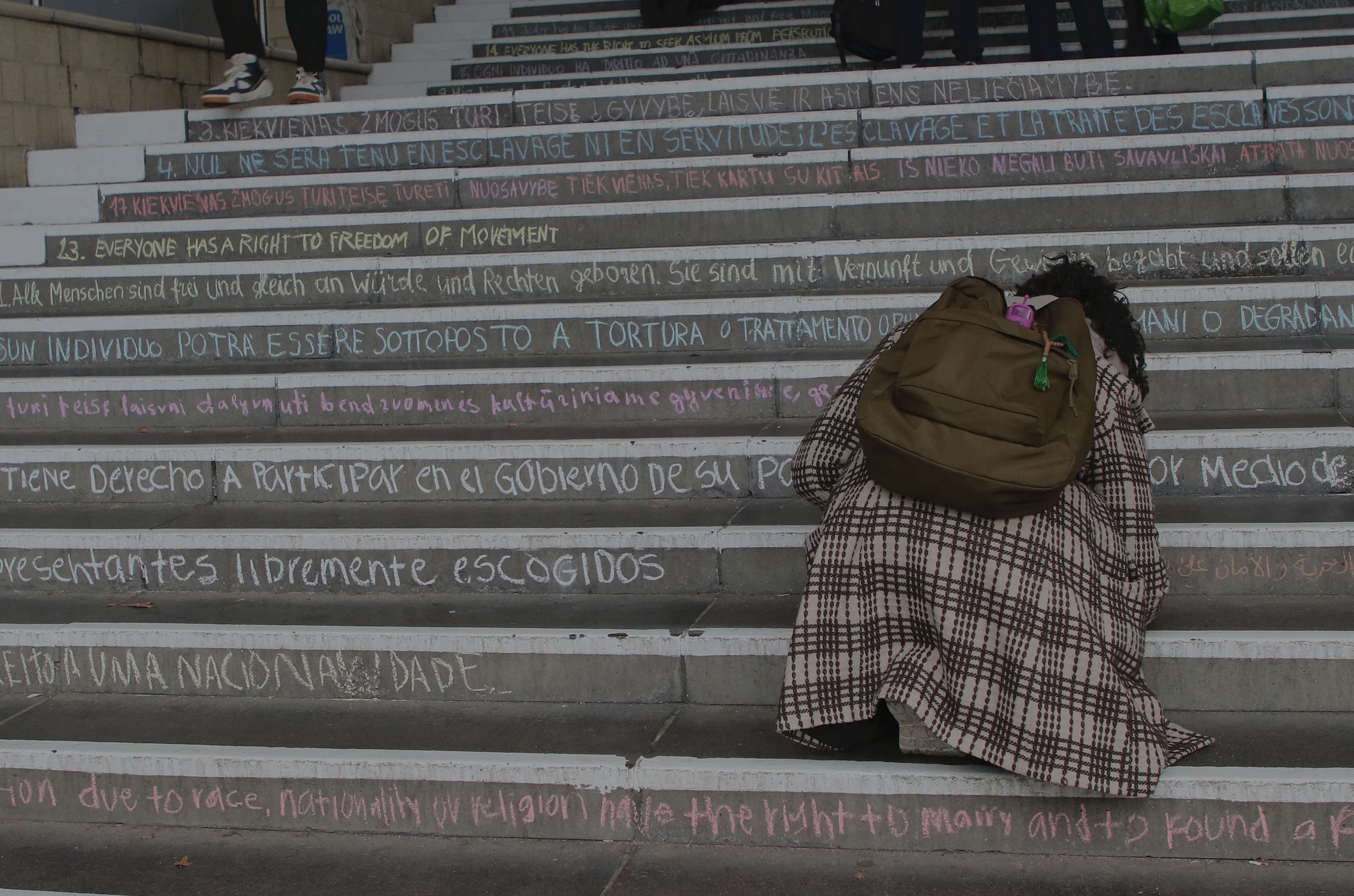
This group of close to half a million people are some of the most vulnerable in society, but they are just the tip of the iceberg. Globally, millions of mental health patients and people living with limited capacity for decision making are at risk from legislation that fails to comply with international human rights standards and practices that fail to properly represent them.
The Essex Autonomy Project, founded in 2010, is helping to change that.
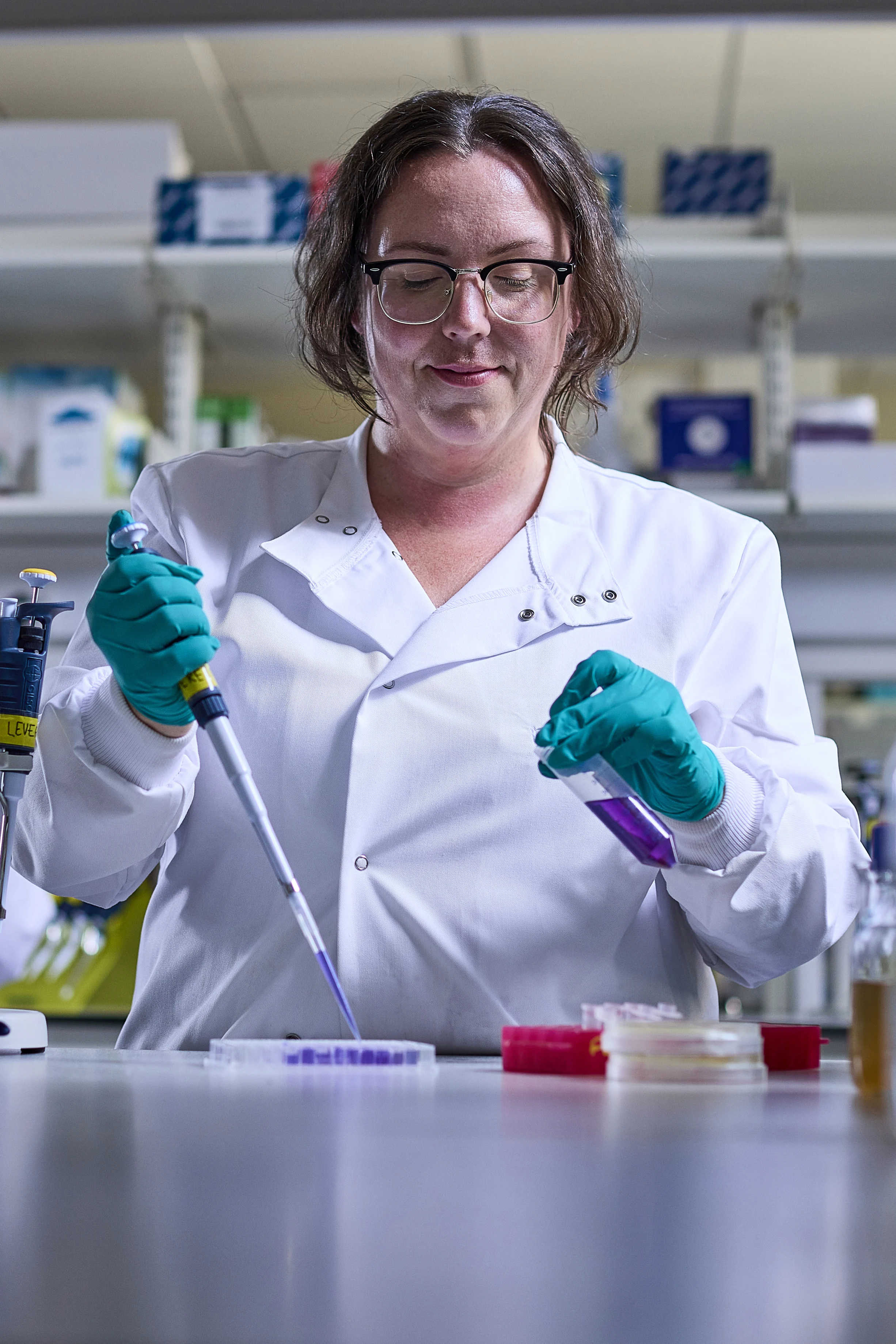
Led by Professor Wayne Martin, the Project team includes philosophers, lawyers, health and social care experts, speech and language therapists, and human rights experts, working with external practitioners and partners.
Together, they are shaping the international debate around human rights and disability.
Their expertise is proving incredibly valuable to policymakers, social workers, lawyers and frontline health professionals.
“We are living through a period of extraordinary change in the practices of care. It is a privilege to help embed principles of autonomy and human rights at the heart of the care relationship.”
Professor Wayne Martin
Director, Essex Autonomy Project


Shaping global health reform
At a meeting in Washington DC in 2016 Professor Martin was surprised to find a group of legal experts from Peru were relying on findings and recommendations made by the Essex Autonomy Project (EAP).
“They told me case studies developed by the EAP team had been used by the Reform Commission for the Civil Code in Peru. They were using our case studies to ‘stress test’ new legal procedures,” said Professor Martin.
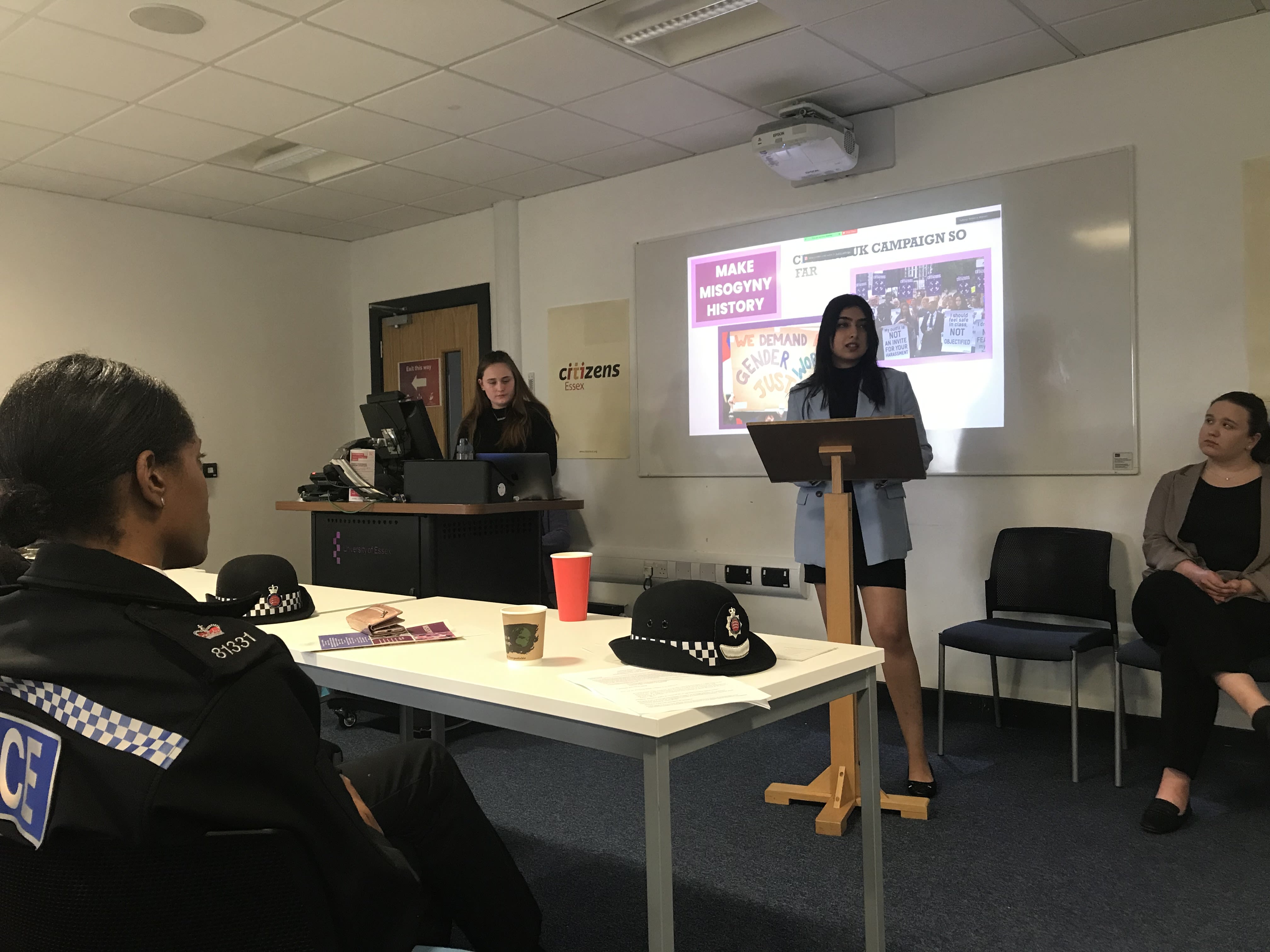
The team was already playing a pivotal role as the UK government wrestled with its compliance with the United Nations Convention on the Rights of People with Disabilities (CRPD), organising vital roundtable discussions at the Ministry of Justice and surveying progress towards CRPD-compliance.
Their recommendations were cited in submissions to the UN where they also presented evidence to the UN Committee on the Rights of Persons with Disabilities.
They hosted the UK’s first public debate on whether the Mental Capacity Act complied with the UNCRPD. Their research provided evidence that the Second Principle of the Act - which states “a person is not to be treated as unable to make a decision unless all practicable steps to help him to do so have been taken without success” - is critical in protecting autonomy, vital to achieving full CRPD-compliance, but poorly implemented in practice.

Applying principles of autonomy to a pandemic

After a decade, the team faced their biggest challenge yet as the COVID-19 pandemic unfolded in 2020, presenting unprecedented challenges.
When a regional NHS Trust wrote to the University with an anxious request, “send us an ethicist”, the EAP team, with its established network of contacts in the care sector and policy community, were ideally-placed to support frontline health professionals.
The initial challenge was to provide a bioethical and human rights assessment of triage principles. What developed was a far-reaching, agile portfolio of research supporting human rights in care delivery during an exceptional crisis.
Professor Martin assembled a multi-disciplinary research taskforce with expertise in bioethics, human rights, medical and equality legislation and care practice.
The team provided research support to an ever-widening circle of professionals, policymakers and public bodies on ethical and human rights issues: supporting NHS Ethics Committees in formulating triage policies for ICU beds; gathering data about training needs in locked-down care homes for the Department of Health and Social Care; and supporting Parliament in considering human rights implications of COVID passports and visitor restrictions in locked-down care homes.
One sustained line of research concerned decisions about Do Not Attempt CPR (DNACPR) recommendations.
DNACPR “mission creep”
In March 2021 the team launched a unique national survey of care professionals working in and with locked-down care homes, followed by a series of focus groups.
What emerged was not only hard evidence about reported “blanket use of DNACPR decisions” but also evidence that care home residents were being denied access to hospital treatment because of the incorrect use of DNACPR recommendations.
“Some residents are being inappropriately denied transfer to hospital or access to certain medicines. The best way to describe it is a form of ‘mission creep’ of DNACPR recommendations being used beyond their intended remit,” explained Professor Martin.
Their findings, published in the British Journal of Social Work, showed that 17% of respondents reported they had witnessed DNACPR recommendations informing care and treatment decisions beyond cardiopulmonary resuscitation. More than half reported that DNACPR recommendations were made without consulting with the individual or their families.
Findings were submitted to the Parliamentary Joint Committee on Human Rights – where Professor Martin later gave oral evidence – and were described by the Special Advisor to the inquiry as “exactly the sort of gritty stuff that is needed to be able to ground recommendations.”
Their recommendations for new standards, guidance and training are already making a difference.
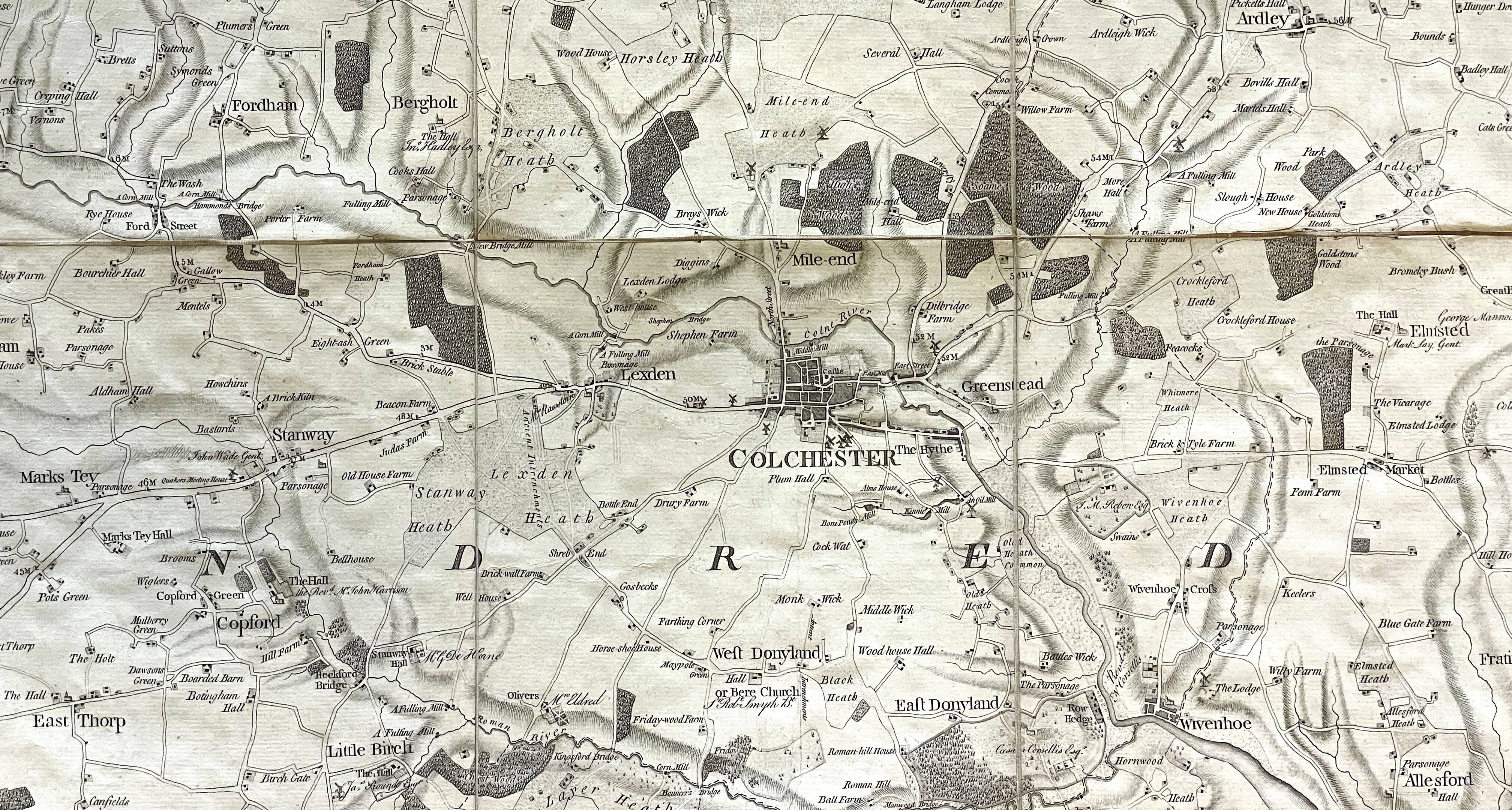
At St Helena Hospice in Colchester, Chief Clinical Officer Dr Karen Chumbley, who is also the Suffolk and North East Essex Integrated Care System Clinical Lead for End of Life Care, has made changes in response to the research.
Dr Chumbley has worked to highlight the importance of individualised decision-making, consultation and advocacy and clear documentation and practice regarding DNACPR decisions. Locally, the integrated care system has implemented the ReSPECT process, in which any decisions about CPR are embedded within a wider, holistic discussion about the person’s priorities for future care.

Changing professional practice through training
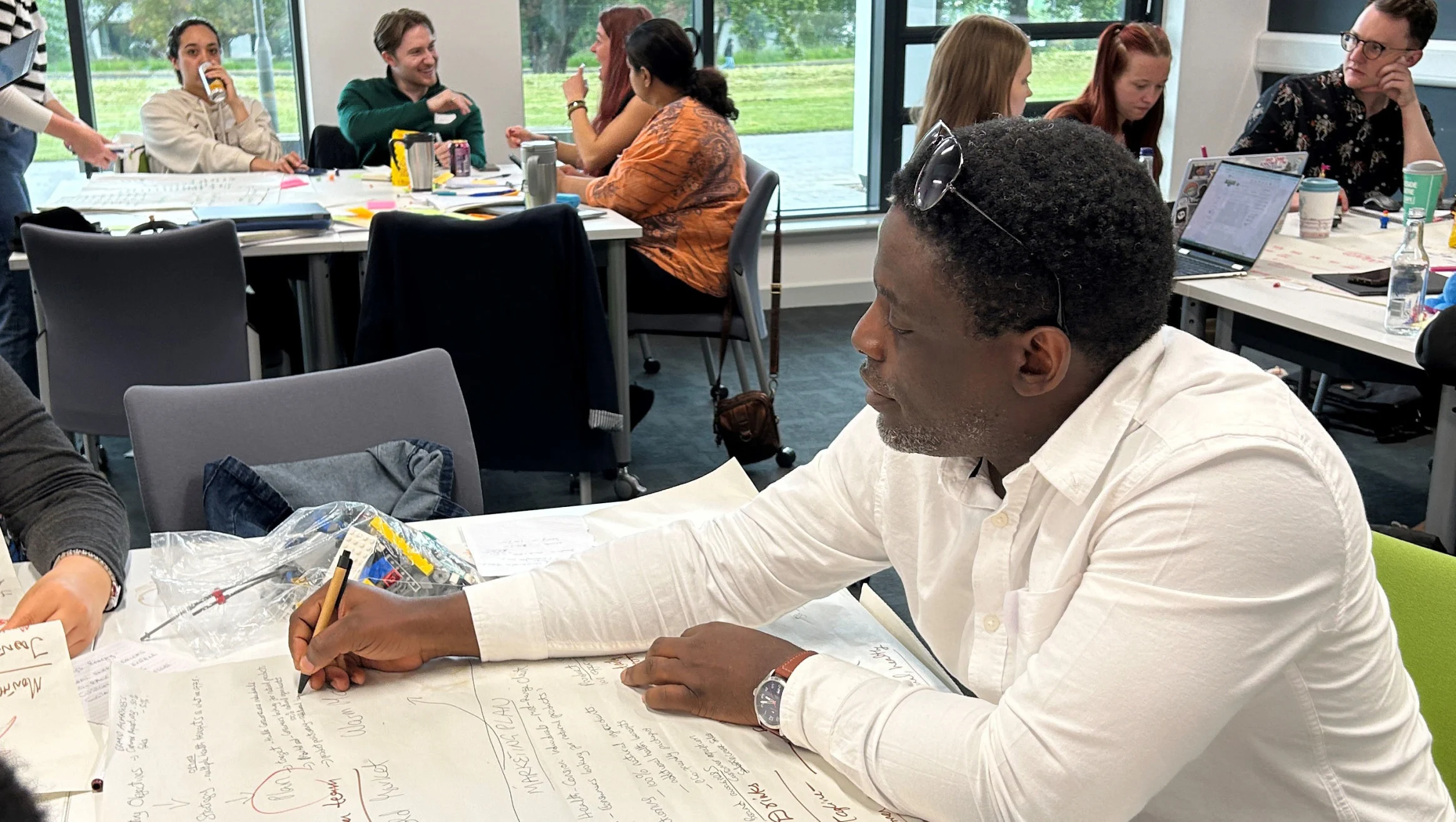
Not content with influencing policy and practice through research, the EAP team is dedicated to delivering comprehensive research-informed training for professionals.
Through summer schools and workforce training they have made practical changes to the way the human rights of those in care are protected.
The summer school has provided an intensive and interactive programme to hundreds of professionals, policymakers, researchers and students.
Participants have described it as an “invaluable space to consider issues away from the immediacy of day-to-day implementation dilemmas” and an opportunity that “brought greater clarity to certain concepts.”

"With an impressive array of topics, it was one part ideas generator and one part travelogue as people from different professions and backgrounds looked through different sides of a prism. Attending the Summer School should feature in the job description of the National Mental Capacity Forum’s Chair."
Dr Margaret Flynn, Chair of the Mental Capacity Forum
Workforce training provides insights on current research, legal developments and ethical issues with collaborative exploration of case study material.
The team has delivered specially-designed training to more than 120 judges through a Judicial College module, hundreds of legal professionals through the Court of Practice Practitioners Association, and thousands of Best Interest Assessors, doctors, mental health professionals and independent mental capacity advocates.
During the pandemic, in partnership with the National Mental Capacity Forum, they delivered ‘rapid response’ webinars each attracting between 500 and 800 care and capacity professionals. As well as providing vital guidance for frontline staff, the webinars enabled the researchers to gather and analyse real-time data about practices and training needs in locked-down care homes. That data informed further guidance developed by the National Mental Capacity Forum, the Department of Health and Social Care, and the Ministry of Justice.
One participant described the researchers as “the only people who understood the daily challenges, dramas, frustration and injustices…in care homes.”

"Those webinars stood the test of time. The impact of this work endures, as it also provides a mine of information for future scholars who wish to understand the pandemic as it unfolded."
Baroness Ilora Finlay, Crossbench Member of the House of Lords
Essex’s vision for rights in care

Achieving recognition for vulnerable, marginalised and sometimes invisible people in care is an incredible challenge which the EAP team see as an exciting opportunity.
In 2006, the global community came together at the UN at the Convention on the Rights of Persons with Disabilities which resulted in a lot of promises. Ever since, Professor Martin and his team have been committed to doing what they can to ensure those promises are kept, but there are always new challenges on the horizon.
Most recently, the team has provided advice to the legal team at MIND, who are posthumously appealing a decision in the case of Sudiksha Thirumalesh. The 19-year-old was denied treatment because of a long-standing legal precedent, the so-called MM Dicta, which state that patients lack capacity if they do not accept their medical prognosis.
With the MM Dicta firmly in their sights, the EAP team remain firmly committed to protecting the rights of patients.
Their dedication has not gone unnoticed.
“Wearing my academic, professional and policy hats, I can say confidently that Wayne and the Autonomy Project have contributed materially, substantially and originally to each of these domains.”
Alex Ruck Keene QC (Hon), Barrister and Special Adviser to the UK Parliament’s Joint Committee on Human Rights (inquiry into Human Rights in Care Settings)


Find out more
Securing rights in healthcare - everything you need to know about training and how the EAP can support you
In Right as Rain: Self-Determination and Autonomy in Health and Social Care, Professor explains why autonomy matters
Sixty Stories
We’re celebrating 60 years of making change happen. 60 years of boldness and bravery from our students past and present. 60 years of creating change.